CASE
A 30-year-old woman presents to the emergency department with left arm pain from a chronic wound. She notes that the wound has been present for greater than a year and it becomes malodorous and painful and oozes intermittently. She reports fevers up to 103 degrees Fahrenheit. She endorses a one-year history of near-syncopal episodes associated with shortness of breath, headache, and neck pain. She reports polysubstance use including fentanyl, xylazine, and cocaine, and has a history of injection drug use and Hepatitis C. Her last hospitalization was one month ago for a similar wound, at which time she received intravenous antibiotics and was subsequently discharged. Two years prior, she reports having a similar wound on her right arm, which required debridement and skin grafting. Due to her drug use, she states that she has visited several medical centers who have denied her surgical intervention for her wounds.
Physical examination was notable for tachycardia. The left upper extremity had a malodorous wound on the left dorsal antebrachium, extending down to the wrist (Figure 1). Complete blood count and comprehensive metabolic panel revealed microcytic anemia, elevated transaminases, and elevated alkaline phosphate. X-ray of the wrist, forearm, and elbow were normal. CT of the upper extremity revealed chronic radial and ulnar osteomyelitis. Cefepime and vancomycin were administered. She was admitted and treated with intravenous antibiotics and skin graft, and was discharged to a rehabilitation facility. Xylazine is a veterinary sedative that has been increasingly implicated in overdose deaths throughout the United States.1-3 It was first reported as a heroin adulterant in Puerto Rico in the early 2000s and again in the 2010s as a drug of its own.4-6
Skin necrosis due to patient using xylazine. (Click to enlarge.)
Since 2020 to 2021, the Drug Enforcement Administration has reported a sharp rise in xylazine use across the U.S., with the first cases beginning in the northeast. Recently, Philadelphia has been reported as having the highest prevalence of xylazine, with xylazine present in 25.8 percent of all overdose deaths in 2020.1 Known by street names such as “tranq,” or “tranq-dope,” oxylazine is increasingly found in patients with opioid overdose.
Brief history of xylazine
The drug was first developed in Germany in 1962 by Bayer as a non-narcotic analgesic and muscle relaxant for animals.6 It is an alpha-2 agonist, similar to clonidine, which inhibits the release of dopamine and norepinephrine in the central nervous system, causing decreased sympathetic activity which results in sedation. In humans, acute intoxication presents with findings typical of an opioid toxidrome, such as miosis, central nervous system depression, respiratory depression, hypotension, lethargy, and coma.7 Xylazine withdrawal may be severe, with agitation, anxiety, or hypertension, and may require inpatient or intensive care treatment.8 Chronic side effects of xylazine may include skin ulcers associated with foul-smelling purulent discharge and associated complications such as soft-tissue necrosis (often extensive), bacteremia, and osteomyelitis.1,9,10 The pathophysiology of skin ulcers is thought to be due to the vasoconstricting effect of xylazine, which causes a chronic state of decreased skin perfusion, impaired wound healing, and subsequent tissue necrosis.
Treatment in patients
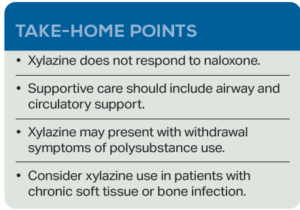
Xylazine should be considered in all patients who present with history of injection drug use and chronic wounds. Initial stabilization includes airway management and circulatory support. Currently, there is no FDA-approved pharmacotherapy for either the reversal of xylazine in humans or the management of withdrawal. Typically, xylazine is mixed with fentanyl. While naloxone can treat fentanyl overdose, overdose symptoms may persist when xylazine is involved.
Workup may include metabolic panel, complete blood count, and imaging in cases where trauma or infection occur. Xylazine is not detected by routine toxicologic studies. Xylazine-induced skin ulcers typically begin as a blackened eschar that progresses to a cribriform appearance.10 The wounds are purulent and often polymicrobial. Many of these infections require hospitalization with intravenous antibiotics and surgical debridement. However, xylazine withdrawal is often so miserable that patients are at risk of leaving the hospital against medical advice before treatment is completed.
 Isha Joshi (@ISHAJOSHIII) is a third-year medical student at Penn State College of Medicine in Hershey, Pa. Prior to medical school, she received her MBA in Healthcare Management and currently works on health policy and outcomes-based research.
Isha Joshi (@ISHAJOSHIII) is a third-year medical student at Penn State College of Medicine in Hershey, Pa. Prior to medical school, she received her MBA in Healthcare Management and currently works on health policy and outcomes-based research.
 Dr. Marco is professor of emergency medicine at Penn State Health Milton S. Hershey Medical Center and the associate editor of ACEP Now.
Dr. Marco is professor of emergency medicine at Penn State Health Milton S. Hershey Medical Center and the associate editor of ACEP Now.
 Dr. Lubin is a professor of emergency medicine and public health sciences and the program director for the MD/MPH dual degree program at the Penn State College of Medicine in Hershey, PA, where he is also the vice chair of research for the department of emergency medicine at the Penn State Health Milton S. Hershey Medical Center.
Dr. Lubin is a professor of emergency medicine and public health sciences and the program director for the MD/MPH dual degree program at the Penn State College of Medicine in Hershey, PA, where he is also the vice chair of research for the department of emergency medicine at the Penn State Health Milton S. Hershey Medical Center.
References
- Friedman J, et al. Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug and Alcohol Dependence. 2022;233:109380.
- Alexander RS, et al. Xylazine and overdoses: Trends, concerns, and recommendations. Am J Public Health. 2022;112(8):1212-1216.
- Love JS, et al. Opioid overdoses involving xylazine in emergency department patients: a multicenter study. Clin Toxicol (Phila). 2023 Mar;61(3):173-180.
- US Department of Justice, Drug Enforcement Administration. The Growing Threat of Xylazine and its Mixture with Illicit Drugs: DEA Joint Intelligence Report. DEA Product Number DCI-DIR-001-23. Available here. Published online October, 2022. Accessed June 16, 2023.
- Reyes JC, et al. The emerging of xylazine as a new drug of abuse and its health consequences among drug users in Puerto Rico. J Urban Health. 2012;89(3):519-26.
- Ruiz-Colón K, et al. (2014). Xylazine intoxication in humans and its importance as an emerging adulterant in abused drugs: A comprehensive review of the literature. Forensic Sci Int. 2014;240:1-8.
- Capraro AJ, et al. (2001). Severe intoxication from xylazine inhalation. Pediatr Emerg Care. 2001;17(6):447-8.
- Gupta R: Xylazine – Medical and public health imperatives. N Engl J Med. 2023; 15;388(24):2209-2212.
- Rodríguez N, et al. GC-MS confirmation of xylazine (Rompun), a veterinary sedative, in exchanged needles. Drug and alcohol dependence. 2008;96(3):290–293.
- Malayala SV, et al. Xylazine-induced skin ulcers in a person who injects drugs in Philadelphia, Pennsylvania, USA. Cureus. 2022;14(8):e28160.
The post Xylazine: An Emerging Threat appeared first on ACEP Now.










